Introduction:
Ankle sprain is the most common type of ankle injury. A sprained ankle can happen to athletes and non-athletes and children and adults. Ankle is the 2nd most commonly injured body site. It is estimated that 80 to 85% of ankle sprains occur to the lateral ligaments. It is generally accepted that an inversion sprain is more severe, with greater instability. However, an inversion sprain is more common, with the lateral ligaments involved in 80 to 85 % of all ankle sprains.
The anterior talofibular ligament (ATFL) is the most commonly injured ligament.
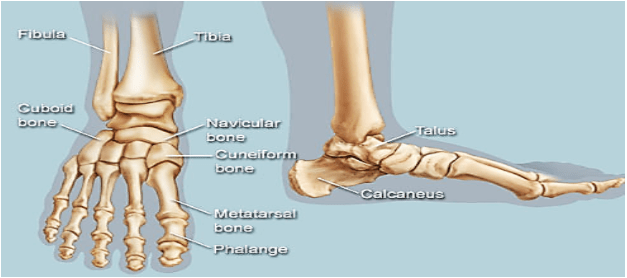
Anatomy:
The ankle complex includes three joints:
Talocrural (ankle) joint
- Synovial hinge joint between tibia, fibula, and talus.
- Inferior tibiofibular joint unites tibia and fibula into mortise
- Talus is tenon within mortise of tibia + fibula
Motion: Hinge joint: Extension (dorsiflexion) and flexion (plantar flexion)
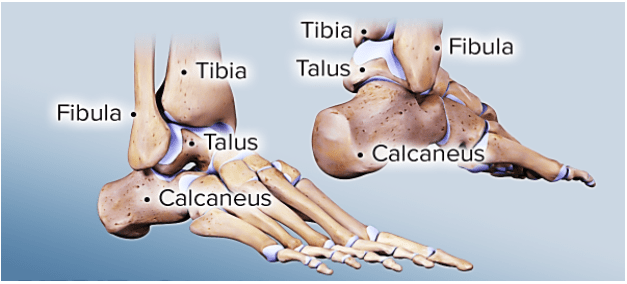
Subtalar joint:
- Synovial joint between talus and calcaneus
- Divided into an anterior and posterior articulation separated by the sinus tarsi
Motion: Inversion, eversion, and anteroposterior gliding
Inferior tibiofibular joint:
Distal parts of the fibula and tibia articulate to form fibrous Inferior tibiofibular joint (tibiofibular syndesmosis).
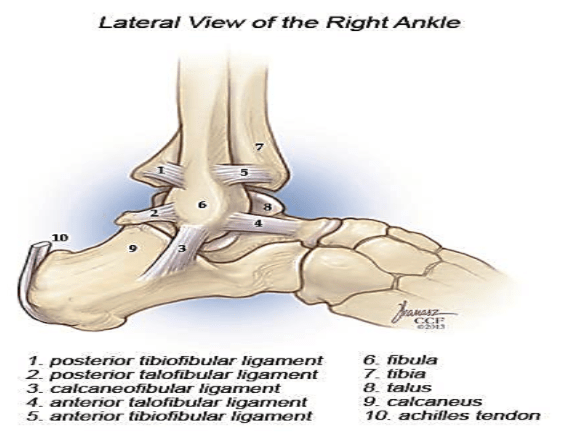
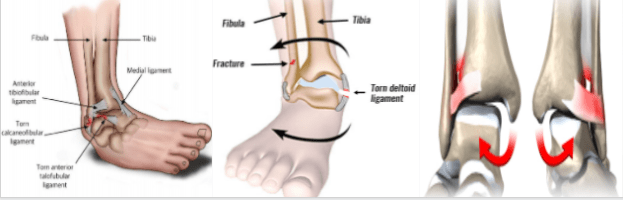
LIGAMENTS
3 sets of ligaments stabilize ankle complex:
- Lateral collateral ligaments
- Medial collateral ligaments (deltoid ligaments)
- Distal tibiofibular syndesmotic complex
Lateral collateral ligaments:
- Stabilize ankle against inversion and anterior, posterior subluxation.
- Anterior talofibular ligament (ATFL): it is the main talar stabiliser. Stabilizes talus against anterior displacement, internal rotation, and inversion
- Calcaneofibular ligament (CFL): secondary lateral restraint of subtalar joint
- Posterior talofibular ligament (PTFL)
- Lateral talocalcaneal ligament (LTCL)
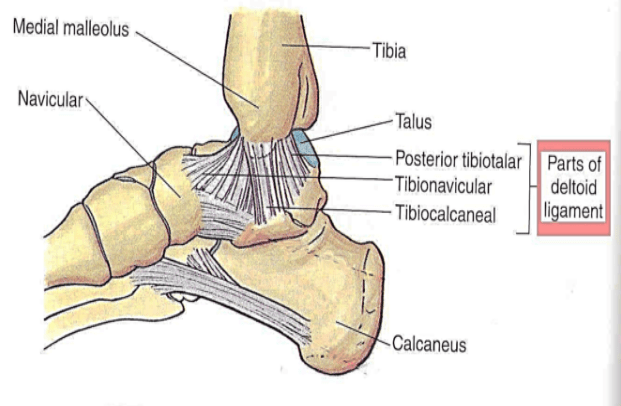
Medial collateral ligaments (deltoid ligament):
- Divided into superficial and deep components
- Superficial: From superficial margin of medial malleolus, provide rotational stability.
- Deep: Posterior and anterior tibiotalar ligaments. prevent joint eversion.
Tibiofibular syndesmotic ligaments:
- Maintain width of ankle mortise, stabilize against eversion
- Anterior and posterior inferior tibiofibular ligaments
- Inferior transverse ligament: Distal to main posterior tibiofibular ligament
- Interosseous ligament: Distal thickening of syndesmotic membrane.
RANGE OF MOTION:
Primary plane motions include:
- Sagittal plane motion: dorsiflexion (15°- 25°) and plantar fiexion (50°-55°)
- Frontal plane motion is inversion (35°) and eversion (20°)
- Transverse plane motion is abduction (10°) and adduction (20°)
- Triplanar motions occurring about oblique axes defined:
- Pronation (20°) is a combination of dorsiflexion, eversion, and abduction.
- Supination (35°) is a combination of plantar flexion, inversion, and adduction.
Classification
Ankle sprain classified in to:
Low ankle sprain:
- Lateral ankle sprain “classic sprain” 80% to 85%
- Medial ankle sprain 5% to 10%
High ankle sprain:
- Syndesmotic sprain 5% to 10%
Lateral ankle sprain:
- The most common mechanism of ankle injury is inversion of the plantar-flexed foot.
- The anterior talofibular ligament is the first or only ligament to be injured in the majority of ankle sprains.
- Stronger forces lead to combined ruptures of the anterior talofibular ligament and the calcaneofibular ligament.
Medial ankle sprain
- The medial deltoid ligament complex is the strongest of the ankle ligaments and is infrequently injured.
- Forced eversion of the ankle can cause damage to this structure but more commonly results in an avulsion fracture of the medial malleolus because of the strength of the deltoid ligament.
High ankle sprain (Syndesmotic sprain)
- Dorsiflexion and/or eversion of the ankle may cause sprain of the syndesmotic structures.
- There generally tends to be less swelling with a high ankle sprain, however there tends to be pain that is more severe and longer lasting.
- Syndesmotic ligament injuries contribute to chronic ankle instability and are more likely to result in recurrent ankle sprain and the formation of heterotopic ossification.
Clinical features:
- Pain (rest and weight bearing)
- Swelling
- Redness , ecchymosis
- Instability
- Weakness
- Impaired proprioception and postural control
- Activity limitation and participation restriction
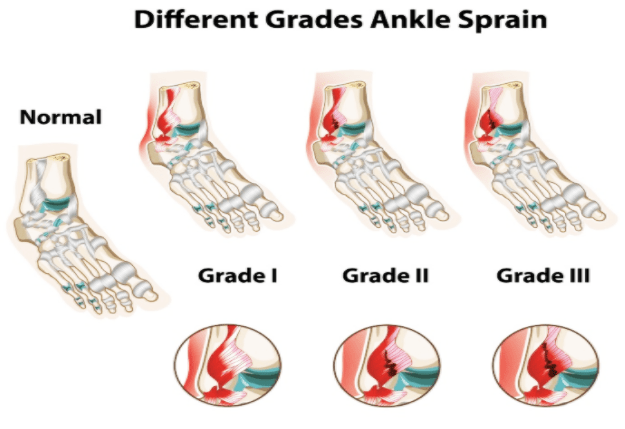
Grading of Ankle Sprain:
Grade I sprain:
- It represents a microscopic injury without stretching of the ligament on a macroscopic level.
- Patients have mild/little swelling and tenderness with little impact on function.
- There is no joint instability on examination, and the patient is able to bear weight and ambulate with minimal pain.
Grade II sprain
- It has macroscopic stretching, but the ligament remains intact.
- Moderate pain, swelling, tenderness, ecchymosis and reduced proprioception, ROM and mild to moderate joint instability.
- Weight bearing and ambulation are painful.
Grade III sprain
- Involves a complete tear of a ligament.
- Patients have severe pain, large swelling, high tenderness, and ecchymosis.
- There is significant mechanical instability on exams and significant loss of function and motion. Patients are unable to bear weight or ambulate.
Assessment
- To assess the degree of instability.
- Grade of ligament damage.
- Identify any reduction in range of motion or reduced strength.
- Identify any other additional or associated injuries such as an avulsion fracture where a piece of bone at the end of a ligament has come away from the main.
History Taking:
- How did it happen?
- Was there any pain at the time?
- Was the pain sudden onset or gradual?
- Was there any swelling and was it sudden onset or gradual? – a sudden swelling often indicates a bleeding into the joint rather than a gradual increase in synovial fluid within the joint.
- Did you hear any noises? – this could indicate ligaments tearing or bone breaking.
- Did you apply any emergency procedures such as RICE?
- Is there anything you do which makes it worse / better?
Physical Examination:
- There is swelling, ecchymosis and tenderness on the affected site.
- The degree of swelling or ecchymosis is proportional to the likelihood of fracture.
- Palpation should include bony landmarks such as the lateral malleolus, medial malleolus, the fibula, the fifth metatarsal and the physis in skeletally immature patients.
- Achilles tendon, peroneal tendons, and posterior tibial t
- endon should also be palpated.
- Tenderness over the anterior joint line or syndesmosis may indicate a sprain of the interosseous membrane.
- Recurrent sprains often have very little swelling.
- An individual with an ankle sprain can almost always walk on the foot carefully with pain.
- Grade III ankle sprains often include an audible snap followed by pain and swelling.
- A careful neurologic examination is essential to rule out loss of sensation or motor weakness, as peroneal nerve and tibial nerve injuries are sometimes seen with severe lateral ankle sprains.
Special Tests:
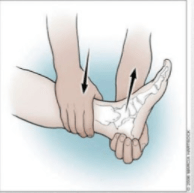
Anterior Draw Test
Purpose: To test for ligamentous laxity or instability in the ankle. This
Test primarily assesses the strength of the Anterior Talofibular Ligament.
Diagnostic Accuracy: Sensitivity: 71%; Specificity: 33%

Talar Tilt test
Purpose: The talar tilt test detects excessive ankle inversion. If the ligament tear extends posteriorly into the calcaneofibular portion of the lateral ligament, the lateral ankle is unstable and talar tilt occurs.
Diagnostic Accuracy: Sensitivity: 67%; Specificity: 75%
External Rotation Stress Test:
Purpose: To help identify the tibiofibular Syndesmotic injury(high ankle sprain).
Diagnostic Accuracy: Sensitivity: 20%; Specificity: 84.5%

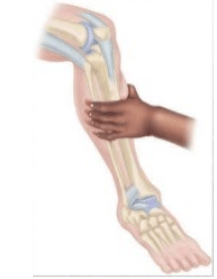
Squeeze (Hopkin’s) Test
Purpose: To help identify inferior Tibiofibular Syndesmotic injury, consisting of compression of the fibula against the labia at the mid-calf level producing pain in the syndesmosis.
IMAGING
MRIs, CT scans, Bone scans, and arthrograms all have diagnostic utility for specific injuries (fractures; avulsions; talar dome fracture) but have little role in the initial evaluation of ankle sprains.
Management:
Conservative Management:
- Initial Management: The initial management of ankle sprain requires the pricier regimen;
P = Protection… crutches, splint or brace
R = Rest…
I = Ice… 20minutes every 2 hours
C = Compression…
E = Elevation …
R = Rehabilitation …
This is probably( the single most important in treatment, particularly with grade I and grade II injuries).
- Pain and swelling can be reduced with the use of electrotherapeutic modalities.
- Analgesics(NSAID) may be required.
Restoring Full Range of Motion:
- The patient may be non-weight-bearing on crutches for the first 24hours but should then commence partial weight-bearing in normal heel-toe gait.
- It will be necessary from this stage to protect the damaged joint with strapping or bracing.
- As soon as pain allows, active range of motion exercises can be performed.
Muscle Conditioning:
- Strengthening exercises should be performed as soon as pain allows.
- Active exercises should be performed initially with gradually increasing resistance.
- Exercise should include plantarflexion and initially with gradually increasing resistance.
Functional Exercise:
- Functional exercises (e.g. jumping, hoping, twisting, figure-of-eight running) should be commenced when the athlete is pain-free, has full range of motion and adequate muscle strength and proprioception.
Treatment of grade III injuries:
- Treatment of grade III ankle injuries requires initial conservative management over a six-week period.
- If the patient continues to make good progress and is able to perform sporting activities with the aid of taping or bracing and without persistent during or following activity, surgery may not be required.
- If, however, despite appropriate rehabilitation and protection, the patient complaint of recurrent episodes of instability or persistent pain, then surgical reconstruction is indicated.
Max. protection phase:
1-3 days
PRICE formula. Protection with a splint. Icing every 2hours during 1st 48hours. Elevation to reduce swelling. Gentle mobilization to inhibit pain. Partial WB with crutches. Muscle-setting Techniques.
Mod. Protection phase:
4-10 days
Non weight bearing AROM. Cross-fiber massage. Grade 2 joint mobilization. Toa curls. Seated calf stretches. Endurance training. Strengthening exercises of intrinsic foot muscles.
Min. protection phase:
11-21 days
Weight bearing as tolerated. Initiate Eccentric exercise. Toe walks. Subtalar mobilization. Tape or Brace for sports or other strenuous activities. Proprioception/balanced board exercise.
Return to activity
3-8 weeks
Weight bearing as tolerated. Agility drills. Advanced Exercise; Static to Dynamic. Isokinetic resistance training. Specific sport training. Protective bracing for participation into a sports.